I am exhausted from being a patient. In the early days of my illness, I kept a journal, tracked symptoms, and made schedules. Now, I cannot be bothered on most days, but recently I have had to re-engage with my medical care due to declining health.
For years, I actively pursued tests that might shed light on why I feel so poorly. One of the most annoying aspects of having ME/CFS is that we look so normal on paper until you start digging into advanced testing. It is a strange place to be, to want positive test results that point to new treatment directions while at the same time hoping that nothing is seriously wrong. If a test comes back positive, I remind myself that knowledge is power. If it comes back negative, I can rule out a condition. Each investigation brings me closer to the truth behind my illness, regardless if it is negative or positive.
Over the years, my strategy has changed. Rather than pursuing medical explanations for each new symptom, I put my head in the sand, hoping it will all go away. Yet new symptoms are usually a harbinger of decline, especially when they settle in permanently. Ignoring symptoms when it gets to this point is rarely a winning prospect.
The new kid on the block – structural diagnoses

I recall the stir that Jeff Wood and Jennifer Brea made when they shared their stories about getting diagnosed with cranial cervical instability (CCI) and, subsequently, occult tethered cord syndrome (OTC). I recently re-read their stories and remembered my initial reaction: this does not apply to me. After all, I have classic ME/CFS triggered by mononucleosis. Twenty years after my initial infection, DNA from the Epstein Barr virus is still detectable in my blood despite grinding away on antivirals for years.
Soon after Jeff and Jen published their stories, my ME/CFS specialist wanted a neurosurgeon to assess me for brain and spine abnormalities, aka the “structural diagnoses.” Given that I have hyper-mobile Ehlers-Danlos Syndrome (hEDS), a genetic connective tissue disease, my altered connective tissue puts me at greater risk for these conditions.
Connective tissue plays a vital role in various structures that support the head and spine, such as ligaments. Likewise, the dura mater (a sheath that houses the brain, nerves, and spinal fluid) and filum terminale (a fibrous thread that dangles from the tip of the conus) are made chiefly of connective tissue.
Bipedalism is especially hard on EDSers. We are like walking Jenga towers – unstable and easy to topple.
I have watched from the sidelines for two years as more people from the ME/CFS community receive these diagnoses and pursue the surgeries to fix them. It makes sense that many people with ME/CFS have structural problems, given the tremendous overlap between hEDS and ME/CFS. According to a new study, 20% of patients attending a set of EDS clinics in the US had CCI, and 40% had tethered cord. These conditions are not rare in people with hEDS.
Falsifiability
I never quite felt at home in the ME/CFS brain+spine community because it seems like I am one of the few people in the various groups who does not want these diagnoses. I realize now that this is not true, and many people with structural diagnoses face an agonizing decision about whether to elect surgery or not. I have had my head in the sand, hoping my ME doctor would forget about it. I recognize the absurdity in my thinking – I do not get to pick and choose what conditions I have. Nor does anyone else.
I understand why people are glad to receive a structural diagnosis in a strange and twisted way (and why they feel gutted when neurosurgeons turn them down). Having a treatable condition is far preferable to having an incurable one with no real prospects on the near horizon.

Rather than seeking one diagnosis that explains most of my symptoms, I try to disprove that I have certain conditions. As a scientist, I was trained that hypotheses must be falsifiable. If multiple diseases can explain non-specific symptoms, this suggests I need more diagnostic testing to narrow the field of possibilities, especially if the stakes are high. But sometimes, there is a lot of ambiguity in medicine, making us rely on clinical diagnoses.
Science also promotes parsimonious thinking – the idea that the simplest explanation is often the best one, aka Occam’s Razor. However, having a multi-system illness has turned this idea on its head. Sometimes the more complex explanations are the correct ones – but they are harder to falsify because there are more variables.
New symptoms appear
In fall 2018, I started having bladder symptoms. I had a peculiar combination of urinary urgency and hesitancy and started seeing a urologist for an interstitial cystitis work-up, but I had bigger issues and dropped the ball. When the symptoms waned, I figured I dodged the bullet.
I did not fully register I was having problems again until my symptoms – mostly hesitancy and loss of sensation – had been constant for at least six months, only this time they were worse and did not go away. When I shared this with my urogynecologist, she shrugged her shoulders and told me I have a neurogenic bladder without doing any further testing. She said I would need to self-catheterize. When I asked her the cause of this new problem, she had nothing more to add.
This past fall, I decided it was time to see a urologist again. I really dislike seeing a new doctor and all that this entails. I swore I would never mention ME/CFS again at new appointments and instead lead with Ehlers-Danlos Syndrome, considering my two leading hypotheses involved EDS. Omitting ME/CFS doesn’t get me much further, but at least they know it’s in my genes, not my head. He seemed dismissive but did order a urodynamics test.
I’ll spare you the gory details, but my test was very abnormal. I could write a separate blog on my urodynamics report, but in short, I have an underactive detrusor muscle, which means I struggle to initiate a stream and get the job done. During urination, the parasympathetic branch of the autonomic nervous system contracts the detrusor muscle via the pelvic splanchnic nerves. So, something must be damaged along that pathway. But why?

When I finally got the green light to void (after they filled my bladder with 700 ccs of fluid), I peed until I no longer had the urge and told the tech I was done. I learned I had only voided 187 ccs, and this was with considerable effort using the diaphragmatic breathing exercises my pelvic floor specialist taught me. The tech pulled another 800 ccs out of my bladder with a catheter. This was an extreme version of what I usually experience, but some days are worse than others. The diagnosis was neurogenic bladder, atonic/under-active type.
Of course, I wanted to know my urologist’s thoughts on why I developed this condition and my prognosis. He showed very little curiosity and said that it is often unknown why people develop a neurogenic bladder, but it won’t improve and will continue to worsen most likely. I got a second opinion from a Stanford urologist, and he towed the same line; the treatment is the same, so why worry about what is causing it? Neither doctor had anything to say about my EDS.
I was offered three options: 1) to self-catheterize (which aggravates another condition I have), 2) to get a sacral nerve stimulator implanted, or 3) to get an appendicovesicostomy, a fancy name for a surgery that involves rewiring your appendix to allow you to pee through your belly button. Fun times! Um, might there be a 4th option?
Time to stop dragging my heels
After I got my urodynamics report, I knew it was up to me to figure out what might be causing my neurogenic bladder. Several conditions can cause an underactive bladder, most of which I can rule out (see table below). The other hypothesis I explored is perineural cysts, but several medical professionals have ruled out their involvement due to their location and small size. I also had an MS workup, and it was negative.
Causes of underactive bladder
| Cause | Status |
| Aging | I am only 52! |
| Neurologic disorders | Hmmm…such as tethered cord? |
| Acute cerebrovascular accidents | No |
| Multiple sclerosis | Ruled out with MRI and spinal tap |
| Parkinson disease | No |
| Injury to the spinal cord, cauda equina, and pelvic plexus | No |
| Pelvic surgery | No |
| Pelvic and sacral fractures | No |
| Herniated disc | No |
| Lesions of the pudendal nerve | ? Doubtful but not checked |
| Infectious neurologic problems | ? Still need to explore this…but no bladder infections |
| AIDS | No |
| Neurosyphilis | No |
| Herpes zoster and H. simplex | Not likely, but do have high IgG titers for H. simplex |
| Guillain-Barre | No |
I figured the most important next step was to get some new MRI imaging done to see if anything had changed since 2017 when I last had one done for a spinal fluid leak study. I went back to Dr. Ian Carroll, who first diagnosed me with perineural cysts, to ask him if this could be the source of my neurological problems. He independently mentioned cervical instability and sent me off with a referral for a lumbar MRI and flexion and extension X-rays. I would have preferred a full head and spine MRI, but beggars can’t be choosers.
Once I had the images, I knew I needed to send them off to a surgeon on the East Coast specializing in EDS and its spinal manifestations. My ME/CFS specialist had been after me for two years to make an appointment with him. I secretly hoped that he would reject my case after reviewing my images, but instead, I got a call shortly thereafter to set up an appointment. So much for wriggling out of this one.
As part of the intake, the doctor required me to do a traction diary. This involved various forms of traction and monitoring a set of vexing head, cervical, and upper shoulder (e.g., paracervical) symptoms I experience. I also completed a lengthy symptom checklist grouped by different conditions. The more checkmarks in the yes column for a category suggests a clinical possibility. He also asked for all imaging involving the spine from the base of the skull to the tailbone, preferably images that optimize visualization of spinal fluid. Then you wait.
If it walks like a duck, quacks like a duck…it is occult tethered cord
This was the first line from my doctor during our video appointment. After toiling away on the traction diary, I expected us to start there. Instead, he came out the gate telling me I had occult tethered cord (OTC) and proceeded to talk about the evidence, the prognosis, the treatment, and what to expect.
Whoa, dude, that was not what I was expecting as the starting place.
The evidence: The term occult in medicine refers to something being concealed or hidden. It means that the condition’s symptoms are present, but the typical signs are not visible. Essentially, it is a clinical diagnosis.
I have several lines of evidence that point to OTC, according to my doctor. The 800-pound gorilla in the room is my abnormal urodynamics test, which he referred to as indicating an extreme neurogenic bladder. I checked “yes” for many of the tethered cord symptoms on his symptom survey. I figured since I don’t have gait problems, pain, or other neurological symptoms associated with tethered cord, something else must be behind my neurogenic bladder. For this doctor, a positive urodynamics test trumps all else.
I also have a few soft signs on my MRI as well. There are many more obvious or “hard signs” in classic tethered cord, such as the presence of a tuft of hair, skin tags, a dimple in the sacral area. A low-lying conus, the tapered lower end of the spinal cord, is also common. Similarly, the presence of a thickened or fatty filum is suggestive. I don’t have any of these findings, apart from a sacral dimple, if you squint.
Instead, I have the following “soft” signs on my MRI. My conus has a posterior orientation, my lumbar spine exhibits a loss of lordosis (loss of curvature), and my neurosurgeon said I have a thin taught filum (the very opposite of a fatty filum). Throw in EDS, and the picture starts looking more like occult tethered cord. Dammit.
The Prognosis: Both of my urologists and the neurosurgeon agree on one thing: my symptoms will not improve, and they will likely progress.
Here is the part that I really don’t like. Tethered cord puts a lot of strain on the spinal cord, and over time, the strain can cause permanent neurological damage. My doctor shared a rather gruesome analogy. Imagine two people: one is punched in the face and knocked out, and the other is someone who is shot in the head. Both people fall to the ground, but only one can get up again. He said the longer you wait to detether, the more likely the nerve damage becomes permanent and cannot be fixed with surgery. Clearly, people with tethered cord want to avoid that.
The Treatment: In my surgeon’s opinion, there are only two options: do nothing, or get a surgery called sectioning the filum terminale or SFT. Interestingly, some patients claim that taking certain peptides and frequency-specific micro-current (FSM) can help, but my neurosurgeon certainly did not mention this. The choice appears to be to get SFT surgery or worsen to the point of no return.
Weighing the evidence
My neurosurgeon has done over 1100 SFT surgeries – an impressive sample size to draw from. I asked him what percentage of the time he cuts into someone’s spine only to find out – whoops – they did not have tethered cord? He said he would ask my question in a slightly different way. What percentage of the time does he perform SFT only to see patients not see any improvements?
He said that number is between 10-15%. And within the set of patients who do not improve, this could be due to them not having tethered cord in the first place or waiting too long for the surgery and having irreversible neurological damage.
When I spoke to my ME/CFS specialist, she told me she regularly meets with my neurosurgeon. She screens her patients for possible structural diagnoses – based on the presence of EDS, symptoms, and an office traction test. Of those, the neurosurgeon agrees to see around half for video consultation. He invites about half of these to do invasive cervical traction, and many of these he sends home without an offer for surgery.
In other words, he is not offering SFT surgery like it is candy. Far from it. He says his job is to demonstrate that people do not have the conditions he specializes in, just as scientists would. He says no to many patients.
In addition to imaging and surveys, he likes to do provocation tests to prove that his patients truly have a structural diagnosis. For OTC, this involves a walking test: walking flat on your feet, walking on your toes, and walking on your heels. The idea is that if you see a provocation of symptoms upon walking on your heels, it adds more weight to the diagnosis. But he told me that the results of my provocation test would not change his mind: he considers me a surgical candidate due to my urodynamics alone.
He also downplays the extent to which surgery will fix me. He thinks that my urinary symptoms will improve and, quite possibly, any provoked symptoms during my heel-walking test. Oddly, the only symptoms provoked when walking on my heels all occur above my waist (dizziness), not below it.
The other aspect that instilled some confidence is that it was the first time I met with a doctor who deeply understands hEDS. As a surgeon, he knows our tissues intimately, and that EDS is a progressive disease. I have pondered hEDS through the lenses of mast cell disease, autonomic neuropathy, dysautonomia, and wear and tear on joints. I had not thought about how altered connective tissue could lead to occult tethered cord. I certainly had not thought about the headache our tissues create for a neurosurgeon. Over the years, he has innovated surgical techniques for people with EDS.
What to do?
I received my OTC diagnosis a few weeks ago and could not talk about it until now. I am still not convinced and find myself playing games, trying to convince myself that the results from my urodynamics were not real, that I don’t have any other symptoms (which is unclear), and that I have a good quality of life, which is a little laughable at this point.
I fear that I will become a Jenga tower – that SFT surgery will be the beginning of the end. One surgery leads to the next, and another, and so forth. My neurosurgeon pointed out surgeries do not necessarily cause the need for other surgeries. Rather, he said EDS is a bit like an onion. You peel away one layer, and there will be others. This is an inherent problem that comes with a connective tissue disease. Stabilizing one region may reveal other unstable areas. Still, this offers me little comfort because I do not want to be in a revolving surgery door.

I have to ask myself what I am afraid of here. I am not opposed to surgery – I have had major abdominal surgery and a C-section. I guess I am afraid of getting surgery for a condition I might not have and ending up with a surgery rewards punch card.
I recently joined a tethered cord Facebook group, and the first post I saw was from a woman who was on her 10th de-tethering surgery. I saw several posts like that and am concerned that the first surgery will lead to subsequent SFTs. This scares the crap out of me because re-tethering typically involves nerve roots adhering to scar tissue, which creates the tether. Except, in this case, the nerve roots are live wires and need to be carefully disentangled from scar tissue without damaging them. I also fear arachnoiditis – a painful condition involving inflammation of the arachnoid membrane layer.
The specter of detethering surgery leading to greater instability in the neck is also something I want to avoid.
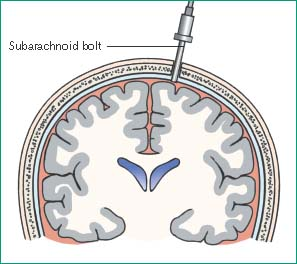
My doctor offered some “appetizers” to go with the main course (my SFT surgery.) to sweeten the deal. He said I could come a day early and get two additional procedures done – invasive cervical traction (ICT) and intracranial pressure (ICP) bolt test. The former involves drilling holes into the skull on both sides and using what looks like an halo or an ice pick to do traction. This is a type of provocation test that allows my doctor to do dynamic measurements. I am not quite sure how this would be helpful at this point beyond intellectual curiosity. It seems like the time to do ICT would be if symptoms worsen after a detethering surgery when the dust has settled.
The ICP bolt test is a dynamic functional test that also involves drilling a hole in the skull and placing a sensor that monitors intracranial pressure. My neurosurgeon thinks that I could have intracranial hypotension that is not necessarily caused by a spinal fluid leak. Tethered cord and perineurial cysts can lower spinal fluid pressure even in the absence of a leak. Given my head symptoms, this might be worth it.
My friend and I joked this would be like a spa week – mani, pedi…and bolts in the skull?
I have yet to decide about the surgery, but I have put a tentative date on the calendar in the distant future while reserving the right to back out. I would love to wait until my condition worsens to see if I really need this surgery, but I do not want to be silly about it and get into the territory of irreversible nerve damage. But I also don’t want to make this decision from a place of fear. No matter what I decide, I know that I am the one who will have to live with the decision, for better for worse.
In the meantime, I will continue to attempt to falsify the hypothesis that tethered cord is causing my bladder symptoms, but I am guessing that the decision ultimately will require a leap of faith.

Hi Caroline, I was detethered in 2017 by Dr Klinge and I’m STILL improving. I’m fortunate enough to have access to supports like PEMF, dry needling, red light therapy, craniosacral therapy, skilled manual physical therapy and Hellerwork. If you are on Facebook please join the group EDS and OTC for more support. Or email me personally.
LikeLike
Thank you so much for writing this. I related to pretty much everything you said. I have been at this forever, I’ve stayed on the bleeding edge of MECFS the entire way, until this. My brain is just filled with noise whenever I even try to investigate this subject. I, like you, have taken things slow. And still am a good few paces behind you.
Thank you for simplifying this process for the layman. Your beautiful breakdown and use of visuals is so much easier to understand than literally anything I have read to date.
LikeLiked by 2 people
I hear you loud and clear. For the past two years, I have had my hands over my ears, my eyes closed while saying lalalalala to block it all out. I want it to all go away. I wish we could find a comfy ledge along the steep cliff face called ME/CFS and live our best days. Sadly, progressive neurological conditions do not usually comply. I wish you all the best in your investigations – give me a shout if you need some support 🙂
LikeLiked by 1 person
Hello Ann – You captured my sentiments very succinctly. The further I dig into something, the murkier it gets. Oh to be OK with taking things our doctors tell us at face value. Sending best thoughts to you.
LikeLiked by 1 person
yes , so well said. i can relate to all that you said. I gad no idea though, that the bladder isues could he tethered cord. I have the exact same bladder issues. This is very unnerving to hear that the damage can get worse.
All the best for you both.
LikeLike
Thank you 🙂 There are many causes of bladder dysfunction/neurogenic bladder. As I said to Christina (in another comment), it is important to rule/out possible causes. People with EDS are more likely to have an impaired filum terminale – it boggles the mind how EDS can cause instability everywhere else in the body and give us an inflexible filum. Go figure! Sending best thoughts 🙂
LikeLike
Wishing you good luck and patience as you make your way along this path.
LikeLike
Thank you, Silvia! Much appreciated!
LikeLike
I’ve got zero words to help you. I’m sorry. You’re obviously very qualified to make this impossible decision (with too many gaps in the data to even enumerate) and I have no input. But I admire you for facing it with such grace, and wanted you to know your openness is valued. My wife faces her own decisions with equal grace. This community is full of pretty awesome people.
LikeLike
Thank you, Kevin. I am so sorry your wife faces similarly tough decisions. My friend and I joke about wanting a weekend off from this job called chronic illness. Sending best thoughts your way.
LikeLike